
Contact us
Our team would love to hear from you.

Like any complex process, RCM requires handling vast amounts of data, where manual operations often lead to delays and errors. Still, one survey found that 62% of U.S. medical practices have automated less than 40% of their revenue cycle operations. Another survey of healthcare leaders revealed that 24% of respondents have never implemented any form of RCM automation. This indicates that automation remains underutilized in healthcare RCM despite its proven benefits.
With rising patient volumes and growing pressure on both healthcare providers and insurers, healthcare organizations need more effective RCM processes to function properly. Below are key reasons why automation is essential.
Medical billing, a core component of healthcare RCM, is both complex and highly repetitive. Manual data entry often leads to errors and denied claims. By integrating with electronic health records (EHRs), hospital management systems (HMS), and other internal management software, automation systems can autofill billing information, assign medical codes, generate claims, and more—reducing errors and ultimately, denials.
Automated systems not only create clean claims from the start, they also validate data before submission, helping them pass through the payer’s system without delays. Eligibility checks are conducted automatically and claims are submitted instantly, eliminating delays caused by manual data entry and verification. These processes shorten the time from care delivery to payment and speed up resolution in the event of denial.
Automated logging of each RCM step makes up-to-the-minute performance accessible to authorized staff members. Standardized, automated workflows also support consistent reporting across departments, clinics, and providers. Automation captures all relevant data across RCM processes, generating insights that support advanced analytics and enable more informed, data-driven decision-making.
The unpredictability, complexity, and lengthy nature of insurance and billing processes often leave patients frustrated. Automation increases transparency and reduces billing confusion by providing timely coverage confirmation, clear upfront estimates, and faster processing. Patients can avoid repetitive paperwork and surprise bills while receiving clear and accurate information about their outstanding balances and claim statuses.
RCM tasks like eligibility verification and payment posting are labor-intensive when performed manually. Considerable time is spent on repetitive data entry, tracking down missing information, and correcting errors. Automation eliminates these tasks, reducing administrative burdens and allowing staff to focus on high-value activities like patient counseling or solving complex denial cases.
RCM automation relies on a combination of advanced technologies, each handling different tasks. Healthcare organizations are increasingly recognizing the benefits of artificial intelligence (AI) and advanced automation for their RCM processes, with 92% of leaders seeing adoption of these technologies as their top priority.

“Manual revenue cycle processes cost time, staff energy, and lost revenue. Automation fixes that with accuracy, speed, and consistent results. Our solutions enable providers to focus on patients while technology handles the complexity of claims and reimbursements.”
Business Analyst
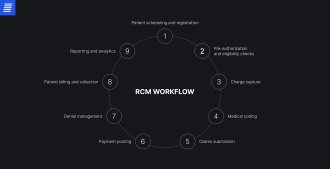
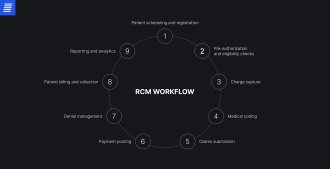
Automation works for almost every step of the financial life cycle of patient care, from registration to payment collection and performance analytics. Following are some prominent examples.
The revenue cycle begins with patient registration, where critical information, such as demographics, insurance, and contact details, is collected to verify eligibility. Errors at this stage lead to downstream denials, delays, compliance issues, and additional costs. Automation captures data and connects with payer systems to confirm coverage in real time. Built-in validation checks detect missing or incorrect data, preventing errors and making this stage quick and efficient.
Medical coding is a key part of the revenue cycle, directly affecting other processes. Although fully automated medical coding is nearly impossible, technologies like AI can significantly streamline the process. This includes providing automated code suggestions to assist specialists, prevent upcoding or undercoding, and ensure alignment with payer rules and industry standards through rules-based support.
As a resource-intensive part of the revenue cycle, claims processing benefits from automation to reduce both processing time and errors. Automated systems create, validate, and submit claims by extracting required information, entering data in accordance with payer rules, and checking for missing details. They also manage status tracking, helping to lighten the workload for medical staff.
A web-based application designed to streamline customer claims processing for a company working in geographically dispersed markets.
In this high-cost area of RCM, automation is essential for efficiency and stronger financial performance. Automated denial management systems detect, categorize, and prioritize claim denials, generate appeals using payer-specific templates, and monitor their status. Powered by ML, these systems can also help prevent denials by analyzing denial patterns and proactively correcting claims.
This RCM stage influences not only cash flow but also patient satisfaction. Automated systems ensure accurate calculation of balances due after insurance adjustments, generate and deliver patient bills promptly, and send reminders for upcoming or overdue bills. With integrated payment, fee collection is also simplified, streamlining the billing process and improving the patient experience.
Automation in revenue cycle management reporting and analytics delivers significant strategic value, giving healthcare organizations the tools to identify bottlenecks and revenue leakage, predict denials, and reduce time spent on manual reporting.
RCM automation is not a simple task, and some challenges require extra attention.
RCM involves handling sensitive patient data subject to strict compliance requirements. Automation must ensure that protected health information (PHI) is collected, stored, transmitted, and processed securely and in accordance with regulations such as HIPAA or GDPR. Our team follows these compliance guidelines and best practices, including end-to-end encryption, access controls, and logging.
Healthcare organizations often rely on multiple, sometimes legacy, systems for RCM—including EHRs, billing, and payer portals—which can make unifying records difficult and slow automation adoption. To enable seamless integration, our engineers standardize and clean data before workflow automation, centralize data repositories, and use interoperability standards such as FHIR and HL7.
Medical and administrative staff may struggle to adopt new workflows, worry that automation could threaten their jobs, and remain skeptical of its accuracy. The solution is to involve personnel early by collecting feedback on system design and addressing their pain points, provide training to help staff embrace the technology and acquire new skills, and keep them involved in high-risk processes.

The EffectiveSoft team focuses on addressing our clients’ underlying problems, closely collaborating with them throughout the development process.
Our team analyzes your current RCM workflow and data quality, identifies pain points, and defines project objectives.
Based on the requirements and objectives, we map out automation opportunities across the revenue cycle, design a prototype, and validate its feasibility.
Our engineers build AI modules, RPA bots, and APIs, integrating them with existing EHRs and other systems while ensuring compliance with relevant regulations and standards, including HIPAA and HL7/FHIR.
Our testing team ensures the system performs as intended while remaining secure and compliant.
Following the Agile approach, we roll out the solution in phases and adjust it based on performance and feedback.
After launch, our engineers provide ongoing support, updating the system to reflect changes in payer rules and regulations, while continuously enhancing its accuracy and efficiency.
Healthcare revenue cycle automation is more than a trend—it’s a critical step toward more accurate records, streamlined processes, and healthier cash flow. By automating RCM processes, healthcare organizations can also reduce the administrative burden on medical staff, freeing up time for strategic tasks and patient care. The first step toward effective automation is partnering with a tech company that knows how to get the job done. At EffectiveSoft, we leverage our expertise in healthcare solutions and the right technologies to deliver tangible results—fewer denials, faster payments, lower operating costs, and more. Contact our team to begin the discovery process.

RCM automation involves applying technology to reduce manual work, improve accuracy, and speed up revenue cycle processes such as eligibility verification, claims processing, and denial management. As a result, staff spend less time on repetitive, manual tasks and can dedicate more time to patients, improving patient care outcomes.
RCM automation influences many healthcare processes, from patient registration to strategy building. Some of the major benefits are reducing errors and inefficiencies, saving costs, and improving patient satisfaction.
Automation is designed to support, not replace, staff. While automation systems cannot handle complex claim denials, communicate with patients, or make strategic decisions, they work alongside staff to streamline processes and achieve better outcomes.
One of the most common technology combinations to achieve automation is RPA and AI, including its subsets, NLP and ML. In healthcare, however, it’s equally crucial to ensure secure data exchange between different systems through HL7/ FHIR APIs.
The primary goals of RCM automation in denial management are to improve claim accuracy, monitor and ensure adherence to payer-specific rules, identify denial patterns, and analyze them to determine root causes. This enables a proactive, preventive approach that lowers denial rates.
In RCM automation, security and compliance depend heavily on proper implementation. At EffectiveSoft, we follow industry best practices, including strong encryption, access control, and auditing, and adhere to healthcare data protection regulations.
Healthcare organizations often face several technical and operational challenges when implementing RCM automation, including system integration, data quality, scalability, and staff resistance. Choosing the right vendor can minimize those struggles. Get in touch with our team to learn more about our approach.
One key RCM workflow automation trend is the expanding role of AI and generative AI. Healthcare providers are moving away from isolated AI use cases to fully intelligent workflows that span the entire revenue cycle. Increasingly, organizations are integrating predictive analytics to proactively prevent denials. Automation adoption is also shaping staff roles, shifting their focus from volume-based tasks to higher-value work.
There’s no set cost, as it depends on multiple factors, such as automation scope, technology stack, integrations, and customization level. Reach out and we’ll walk you through a cost estimate tailored to your requirements.
The time frame for RCM automation depends on project scope, complexity, integration needs, data quality, and more. While a small-scale task takes about two months, enterprise-wide automation may take over a year to implement. To get a project estimate for your specific needs, contact our team.
Can’t find the answer you are looking for?
Contact us and we will get in touch with you shortly.
Our team would love to hear from you.
Fill out the form, and we’ve got you covered.
What happens next?
San Diego, California
4445 Eastgate Mall, Suite 200
92121, 1-800-288-9659
San Francisco, California
50 California St #1500
94111, 1-800-288-9659
Pittsburgh, Pennsylvania
One Oxford Centre, 500 Grant St Suite 2900
15219, 1-800-288-9659
Durham, North Carolina
RTP Meridian, 2530 Meridian Pkwy Suite 300
27713, 1-800-288-9659
San Jose, Costa Rica
C. 118B, Trejos Montealegre
10203, 1-800-288-9659