Contact us
Our team would love to hear from you.


“We understand that every denied claim results in payment delay. That’s why we design systems that give healthcare organizations the visibility, automation, and control they need to get paid faster, reduce administrative burden, and define and eliminate bottlenecks in the collection process.”
Account Manager
Claim denial management in medical billing starts with identifying the root causes. By knowing what leads to denials, healthcare organizations can develop effective mitigation strategies. Below are some of the typical causes.
In a survey by Experian Health, 46% of respondents cited missing or inaccurate data as a leading cause of claim denials. Other reasons include outdated insurance information or patient demographics, incorrect policy numbers, misspellings, inaccurate identifiers, or gender mismatch. These issues cause administrative delays, higher costs, patient frustration, and legal risks.
When healthcare services require prior approval from the insurance company, several issues can lead to claim denials. One of the most common is providing services without obtaining the required prior approval from the insurer. Other issues include invalid or expired authorization, authorization for the wrong procedure or service location, or using a provider not authorized under the plan.
While medical coding plays a key role in correct and timely billing and reimbursement, it is also prone to errors. Common causes of coding errors—such as human error, outdated coding systems, upcoding, and downcoding—can be mitigated through thorough documentation, advanced coding software, partial or full automation, and regular coding audits.
These issues stem from questions regarding whether the service and provider are covered by the patient’s insurance plan. The coverage could be inactive, expired, or exclude the specific service or clinic. Addressing eligibility issues requires a combination of proactive prevention, integration of real-time eligibility verification, and automated workflows for eligibility denials with reporting and analysis.
Claims submitted more than once for the same patient, service, provider, and date of service are detected as unnecessary or erroneous and denied or rejected automatically. Duplicate claims occur due to inadequate claim tracking, system errors, human errors, lack of standardized follow-up process, or insufficient communication between departments. Automation, regular claim status checks, and improved visibility can minimize these issues.
Most insurers have a strict time limit for claim submission or resubmission. Failing to meet this limit leads to an automatic claim denial, regardless of the medical necessity or claim accuracy. If a patient has multiple insurance policies, errors in coordination of benefits (COB), such as failure to determine which insurer pays first, also lead to deadline violations. To deal with this issue, organizations can implement automated alerts, claims tracking systems, and more.
Effective denial management is more than just a necessity. It offers healthcare organizations numerous benefits.
Establishing a comprehensive denial management system requires more than just skills and knowledge—it demands the expertise and tools to handle challenges of any complexity.
One of the most labor-intensive and error-prone processes in RCM is medical coding. Regular coding updates, code mismatches, and entry mistakes all contribute to denied claims.
Applying our deep knowledge of key medical coding systems like ICD-10 and CPT, we create intelligent coding assistance tools. Our experts integrate advanced technologies like AI that can suggest codes and flag common coding errors or unbundling issues. Real-time coding validation ensures the provided services are billed according to payer-specific rules, minimizing the chance of claim denial.
Medical records contain crucial information for denial management, supporting medical necessity for a particular service. However, maintaining these records and ensuring their completeness and accuracy is a difficult task.
To address the challenge of inefficient documentation, EffectiveSoft builds structured documentation templates, ensuring the right fields are completed with precision and accuracy. We integrate real-time documentation quality checks and alerts for missing or incomplete information, enabling healthcare organizations to promptly resolve issues. Seamless electronic health record (EHR) integration for automated filling of necessary clinical and administrative data also helps reduce errors and denials related to inefficient documentation.
When submitting claims, healthcare organizations should follow both payer-specific requirements and regulatory standards. Each insurer has its own timelines and procedures, which can be complicated to work through. At the same time, legal regulations can shift, increasing the risk of claim denials.
We integrate APIs directly at the point of care to automate eligibility and authorization checks. Our denial analytics dashboards provide visibility into trends by denial type, payer, and other key aspects. Alert systems for policy updates and regulation changes help healthcare organizations stay compliant, streamline claims processing, and improve reimbursement rates.
Outdated software and manual processes fail to comply with payer and regulatory obligations and meet the demands of healthcare organizations. As a result, more time and resources are consumed in addressing claims and denials.
To modernize denial management systems, we start by creating automated denial workflow engines with claim routes, prioritization, and progress tracking. Our AI experts implement predictive models for claim denials with recommended preventive actions. We design real-time dashboards and reporting to help healthcare organizations monitor denial rates, appeal success, turnaround time, and recovery rates.

EffectiveSoft enables denial management services through advanced software systems, taking a holistic approach to system design and implementation. Our goal is not just to create a functional tool, but to address the underlying pain points and challenges that healthcare providers face.
Our team evaluates the existing architecture and systems to ensure compatibility, scalability, and seamless integration.
We identify gaps, inconsistencies, and inaccuracies in current datasets for more accurate reporting and root-cause analysis.
Based on the insights we uncover, our specialists create a user-centric prototype of the system, ensuring intuitive navigation and compliance.
Our engineers clean and organize historical and real-time data to support predictive analytics and denial pattern recognition powered by AI and machine learning (ML).
We choose the tech stack that aligns with your security and performance requirements, as well as regulatory standards.
Our team implements the denial management system and performs functional and usability testing, ensuring reliability and accuracy.
Post-deployment, we provide continuous monitoring, updates, and enhancements based on user feedback, evolving needs, and changing regulatory requirements.
Healthcare organizations are already choosing more effective and sustainable solutions to enhance their denial management strategies. Here are the key trends:
We developed a management system for enhanced medical billing and insurance claim submission and processing.
While some healthcare organizations are only beginning their journey to efficient denial management, others have already solved some claim denial challenges.
Over the past decade, MetroHealth, a U.S. nonprofit healthcare system, experienced a rise in payer denials caused by sources across the revenue cycle. The organization also had difficulty identifying the root causes of denials and maintaining transparency across departments.
To address these challenges, MetroHealth partnered with a major RCM solution provider. Through automation, they established efficient workflows to identify root causes and track and investigate unresolved claims. The solution also enabled the organization to analyze any stage of the revenue cycle, improve processes, and prevent denials.
The combined effort cut denials by 30%, unlocking $13 million in revenue over one year, and improved productivity by 8% through automation.
Another large U.S. nonprofit health system, Intermountain Health, sought to reduce medical insurance claim denials while improving patient care. The organization integrated advanced technology and healthcare data analytics into its review process, which reduced manual tracking and enhanced cross-department collaboration.
By implementing a claim denial monitoring tool and strengthening its peer-to-peer review process, Intermountain Health overturned more than $20 million in denials over two years and projected an additional $35 million in revenue.
For healthcare organizations, efficient denial management is more than simply recovering lost revenue; it involves creating a proactive system to prevent claim denials, streamline reimbursement, improve cash flow, and establish sustainable financial performance. With an experienced tech partner and strategic use of advanced technology, providers can turn their financial management from reactive turmoil into a well-balanced, secure process. Contact the EffectiveSoft team to discover how we handle RCM inefficiencies, and let’s strengthen your revenue cycle performance.

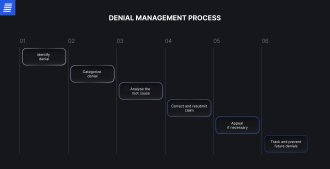
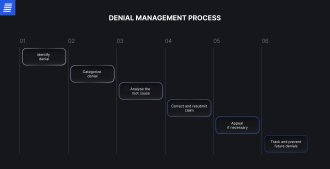
Denial management encompasses the detection, analysis, and resolution of denied insurance claims to guarantee reimbursement for provided services. This process influences the entire revenue cycle and involves not only handling existing denials but also preventing future denials.
Preventing medical claim denials involves a multistep process, beginning with root-cause analysis. By understanding why their claims get denied, healthcare companies can better adjust their processes. Key strategies also include enhancing coding accuracy through staff training and technology assistance, creating standardized processes and documentation, automating eligibility verification, and improving the prior authorization process. Integrating technologies like AI is a key step toward more efficient denial prevention.
Outsourcing denial management can be beneficial for medical companies aiming to strengthen their revenue cycle and reduce claim denials. By partnering with a specialized technology service provider, healthcare organizations can achieve faster and more effective denial resolution through industry expertise, proven best practices, and advanced data analytics. This also helps reduce administrative burden, enhance compliance with payer policies and industry regulations, and cut costs associated with hiring, training, and maintaining an in-house denial management team.
A revenue cycle management system deals with analyzing, preventing, and resolving insurance claims denials. To support its optimal performance, we start with a thorough assessment of each client’s IT infrastructure and requirements to identify the most suitable technologies and tools. To enhance automation and intelligence, we integrate AI, ML, robotic process automation (RPA), and other advanced solutions. For analyzing and reporting, our experts rely on powerful business intelligence platforms like Power BI and Tableau. We also ensure full compliance with industry regulations and healthcare data exchange standards, including HL7 and FHIR, while building secure, compliant infrastructures tailored to our client’s needs.
Effective denial management in healthcare ensures that documentation and claim handling align with industry standards and regulatory requirements, such as HIPAA or GDPR. By tracking, reviewing, and analyzing denials, healthcare organizations can identify systemic issues, implement process improvements, meet documentation standards, and ensure audit readiness. This approach promotes compliance and minimizes the risk of regulatory penalties.
Can’t find the answer you are looking for?
Contact us and we will get in touch with you shortly.
Our team would love to hear from you.
Fill out the form, and we’ve got you covered.
What happens next?
San Diego, California
4445 Eastgate Mall, Suite 200
92121, 1-800-288-9659
San Francisco, California
50 California St #1500
94111, 1-800-288-9659
Pittsburgh, Pennsylvania
One Oxford Centre, 500 Grant St Suite 2900
15219, 1-800-288-9659
Durham, North Carolina
RTP Meridian, 2530 Meridian Pkwy Suite 300
27713, 1-800-288-9659
San Jose, Costa Rica
C. 118B, Trejos Montealegre
10203, 1-800-288-9659